
What's New
- A case study of Exemptia in Hidradenitis Suppurativa published in IJDVL Read More..
- A case of relapsing polychondritis with laryngeal stenosis successfully controlled with Exemptia’ accepted in Indian Journal of Rheumatology.



Select Condition
Select Condition
Tell your doctor about all of your health conditions, whether you:
Also tell your doctor about all the medicines you take. You should not take Exemptia (adalimumab) with abatacept, anakinra, infliximab, etanercept, certolizumab pegol, or golimumab. Tell your doctor if you have ever used rituximab, azathioprine, or mercaptopurine (6-MP).
Exemptia can cause serious side effects, including:
Exemptia is given by injection under the skin.
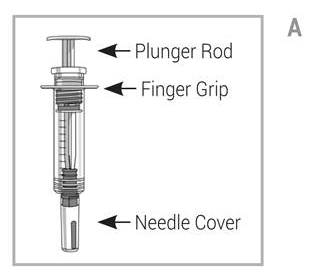
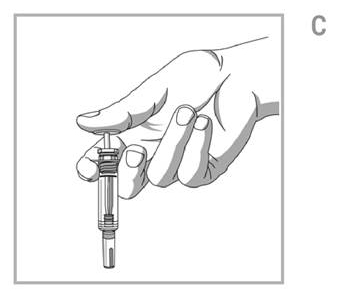
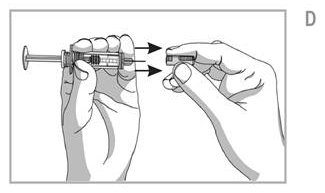
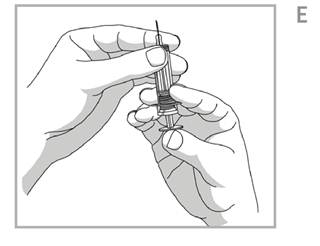
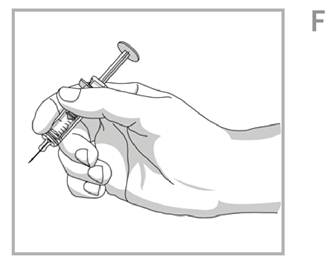
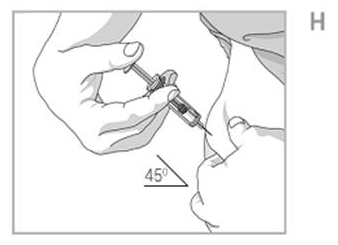
Do not try to inject Exemptia (adalimumab) yourself until you have been shown the right way to give the injections and have read and understood this Instructions for Use. If your doctor decides that you or a caregiver may be able to give your injections of Exemptia at home, you should receive training on the right way to prepare and inject Exemptia (adalimumab). It is important that you read, understand, and follow these instructions so that you inject Exemptia (adalimumab) the right way.
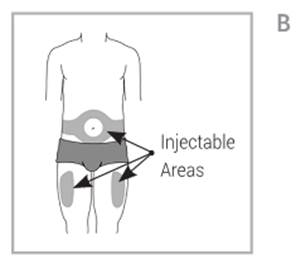
Choose the injection site: wash and dry your hands well. Choose an injection site on:
Prepare the injection site:



Keep a record of dates and location of your injection sites. To help you remember when to take Exemptia (adalimumab), you can mark your calendar ahead of time.
We would be happy to help you find the relevant tools and resources to help you in your Exemptia treatment
Patients and their care givers can enrol in our patient care services to avail our services or get responses to their queries:We know that you are very busy and remembering when to take your Exemptia (adalimumab) medication isn’t always easy. Exemptia CARE offers medication reminders the way that’s most convenient for you. Messages arrive on one day prior to the date you specify for taking the next dosage of Exemptia (adalimumab) and a call comes one day after the date on which you have set up the medication reminder. Plus, you can change your reminder settings at any time by calling. It’s at no additional cost to you.
The cracking sound is related to the rapid shift of fluid within the joint from one space to another and also to changes within the joint cartilage. During flares, the amount of fluid in the joint space increases; as you move, the snapping of irregular, inflamed tissues can create those cracking and popping sounds. Although it can be annoying, it’s not something to worry about. The best way to put a lid on the noise is to continue to keep RA under control with medication and lifestyle changes.
NO. Rheumatoid arthritis is an autoimmune disease, which means your body attacks itself. The target is the synovium, the soft lining around the joints. The immune system sees the synovium as a threat similar to a virus or bacteria and attacks. As a result, fluid accumulates around the joints. The fluid build up causes pain, stiffness, tenderness and inflammatory symptoms of RA. Osteoarthritis, the most common form of arthritis, is a degenerative joint disease. People with OA experience a breakdown of the cartilage that cushions the joints. The wearing down of cartilage causes your bones to rub against each other, which accounts for pain and inflammation. Osteoarthritis does not involve the immune system as in the case of RA.
If you have arthritis, you may be among those people (and there are many) who feel that their arthritis pain is influenced by the weather specifically, that they experience more arthritis pain on cold, rainy days and less arthritis pain on warm, dry days. But research studies on whether climate really does affect arthritis pain have produced conflicting results.
One of the hardest things about having RA is that you never know when symptoms will flare up. If you’ve gone a long time without one, it can come as a shock. During flares, some people feel frustrated and wonder if they did something wrong. So, let’s clear the air at the start. No one can predict when and why flares occur. It’s not your fault. The best way to keep flares at bay is to take your RA medications consistently. But there are some things you can do to reduce the odds of a flare.
On days when you are feeling good, you may be tempted to catch up on all the things you haven’t been able to get done. But be careful not to overdo it. Overdoing activities can bring on fatigue and trigger a flare. On good days, prioritize what needs to be done and pace yourself. Take frequent rest breaks even if you aren’t feeling particularly tired. Ask for help.
Overusing a joint can trigger painful symptoms and cause more damage. You can help protect your joints in a few key ways.
It’s so easy to forget, and yet taking your RA medications at the same time every day is the most important thing you can do to prevent a flare. A regular schedule helps you keep a constant, effective level of medication in your blood. Skipping doses can trigger a flare. So use a pill box, a calendar, or an alarm to help keep you on track. If, despite everything, you feel a flare coming on, call your doctor right away. Your doctor may be able to tweak your medications to help keep RA symptoms during the flare under better control.
NO, there is no cure for RA, but new effective drugs are increasingly available to treat the disease and prevent deformed joints. In addition to medications and surgery, good self-management, including exercise, are known to reduce pain and disability.
Experts disagree whether rheumatoid arthritis affects fertility, but it’s been proven that women with RA do take longer to conceive. This could be chalked up to the side effects of the disease for women, such as low sex drive, inconsistent ovulation, fatigue, and pain. One thing to be aware of is that the medications you might be on for RA may cause birth defects, so you have to work with your doctor to monitor medication if you’re trying to conceive. The minute you and your partner are ready to start trying for baby, see a rheumatologist. Some medications take a month to two years to wash out of your system before it’s safe to conceive. (By the way, that goes for both men and women being treated for RA.) Your rheumatologist will also work out a treatment plan for you while you’re pregnant. Some patients quit medication. Although some women with RA run a slight risk of miscarriage or giving birth to a low-weight baby, the majority of them have normal births without complications. Ironically, 70 to 80 percent of women claim that RA symptoms improved during pregnancy. Another thing to know is that you can’t pass on the disease to your fetus. Though RA has a small genetic component, it doesn’t damage the fetus nor does the baby inherit the disease.
YES. Research suggests that RA symptoms improve during pregnancy, but symptoms usually return and flares can occur after the baby is born. If you have been diagnosed with RA and you are pregnant or plan to be pregnant soon, talk to your doctor about your medications. Some RA medications are not considered safe during pregnancy, and you may temporarily have to stop taking them. Some medications can also affect fertility in both men and women. Ask your doctor which medications are safe to take when breastfeeding.
People with rheumatoid arthritis have a slightly greater chance of having a heart attack or stroke. The risk is probably reduced by controlling the disease, for example with drug treatments. High cholesterol and smoking increase the risk, so it’s a very good idea to eat a balanced diet and stop smoking.
Surgical treatment for rheumatoid arthritis is used to relieve severe pain and improve function of severely deformed joints that don’t respond to medicine and physical therapy. Total joint replacement (arthroplasty) can be done for many different joints in the body. Its success varies depending on which joint is replaced.
Joint surgery often restores near-normal movement in a person who has osteoarthritis in just one or two joints. But this is not the case for people affected by rheumatoid arthritis.
Hoarseness can indeed be related to your RA. Although many people aren’t aware of it, the throat contains cartilage that can become inflamed during a flare. The swelling can affect your voice and even impair your breathing. Mention this symptom to your rheumatologist, and in the meantime, stay clear of smoky areas and try not to strain your voice.
There is no evidence whatsoever that tanning beds have a favorable effect on RA symptoms. In fact, depending on what medications you’re taking, your condition may actually be worsened when you’re exposed to UV rays. Besides, certain RA medications may increase the risk of skin cancer.
Research has also suggested that eating foods rich in omega-3 fatty acids, such as fish, can help reduce inflammation in your body. If you drink alcohol, do so in moderation. If you notice certain foods seem to increase the swelling in your joints, try to avoid them. Maintaining emotional health: You can also improve your physical health by improving your emotional health. High levels of stress might increase your tendency to experience flares and might make it more difficult to deal with the challenges of living with RA.
Sometimes, you might find yourself feeling frustrated or sad about some of the challenges you face when living with RA. Tasks that used to be simple might now be difficult or might require the help of others. Some days, pain and fatigue might leave you feeling helpless or overwhelmed. It’snormal to feel this way, especially at first. It can help to seek support from friends and family ortake extra time to do things that make you happy. You might want to find a support group or online message board for people with RA.
Together with your doctor, you will want to track the health of your bones. You may want to ask your doctor whether you should take a bone density test. Many people with RA develop osteoporosis, a condition in which the bones become brittle and easy to break. This is especially true if you take large doses of corticosteroids, such as prednisone, over a long period of time. There are several steps you can take to help prevent osteoporosis: